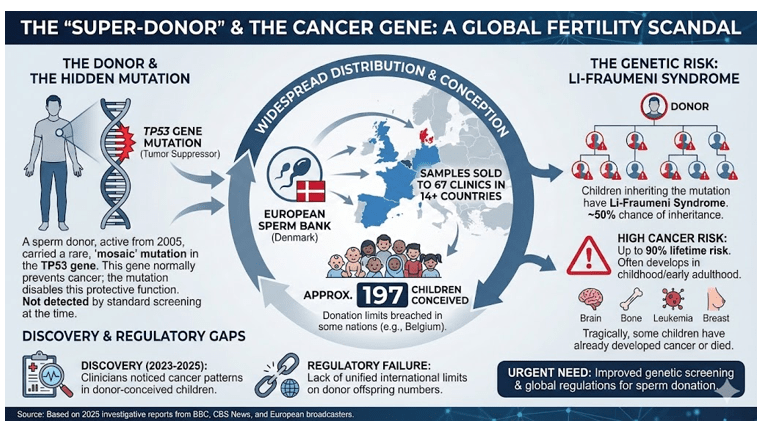
A collaborative investigation by 14 European broadcasters uncovered an alarming situation. A sperm donor unknowingly carried a rare genetic mutation linked to cancer. His sperm reached fertility clinics across multiple European nations. Nearly 200 children were born using his samples over a 17-year period.
The donor possessed a mutation in the TP53 gene. This gene normally prevents cells from becoming cancerous in the human body. His condition caused Li-Fraumeni syndrome, elevating cancer risk by 90 percent. Despite carrying this mutation, the donor remained in good health throughout his life.
The Mutation and Its Transmission
Around 20 percent of the donor’s sperm contained the harmful TP53 mutation. Children conceived using affected sperm inherited the mutation in every single cell. This genetic inheritance guaranteed they would develop the condition affecting their entire bodies. Scientists estimate that most who inherit the mutation will develop cancer during their lifetimes.
The European Sperm Bank in Denmark accepted this donor in 2005. He was a student at the time of his initial donation. Standard screening procedures failed to detect his rare mutation. The mutation proved too uncommon for routine genetic testing at that period in medical history.
The sperm donor scandal
Widespread Distribution Across Continents
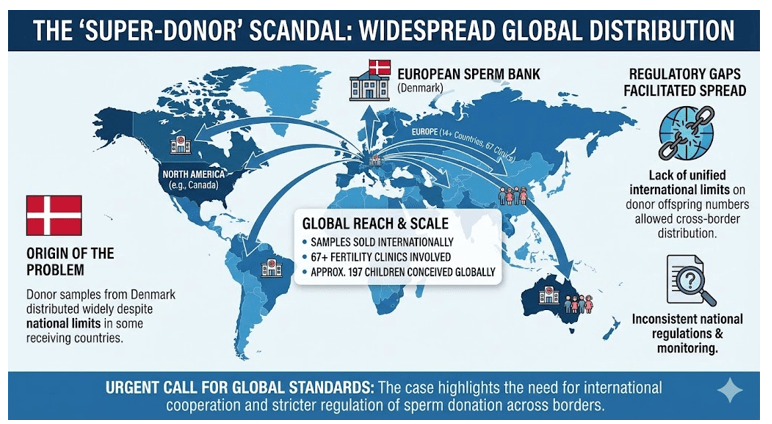
The sperm bank distributed samples to 67 fertility clinics across 14 different countries. Denmark alone accounted for 99 children fathered by this single donor. Belgium reported 53 children born to 38 different women from his samples. This exceeded Belgium’s legal limit by significant margins.
Belgium restricted single donors to conceiving no more than six families. Spain, Greece, Germany, and other nations also received his sperm samples. Ireland, Poland, Albania, and Kosovo clinics obtained samples as well. Sweden had families using his sperm for fertility treatments.
Global distribution of the sperm
When the Problem Surfaced
Doctors discovered the issue in 2020 initially. A child conceived through the bank’s donations developed cancer. That child carried the TP53 mutation in genetic testing. The bank examined a sperm sample following this discovery. Initial screening failed to identify the uncommon mutation at that time.
The European Sperm Bank resumed distributing the sperm after initial testing. Three years later, another child from the same donor developed cancer. Subsequent testing finally confirmed the donor carried the dangerous gene. The bank halted distribution in late October 2023 immediately.
Cancer Cases Among Affected Children
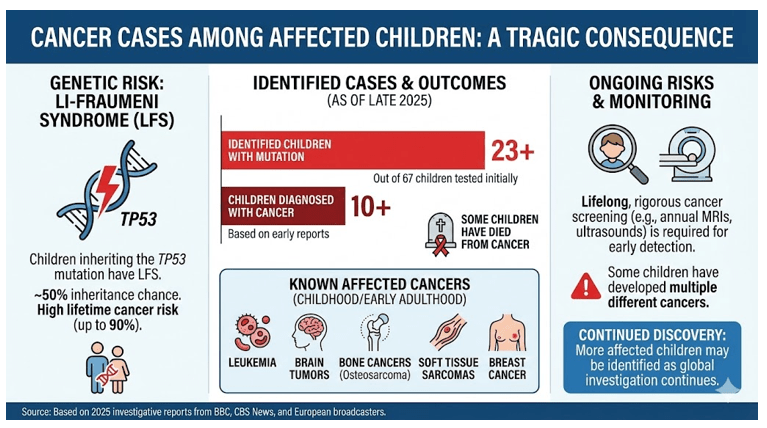
Some children have already died from cancer-related complications. Doctors presented findings at the European Society of Human Genetics conference in May. Out of 67 children identified at that time, 23 carried the mutation. Ten children had already received cancer diagnoses by that point.
Children diagnosed included those with brain tumours and Hodgkin lymphoma. The mutations caused various cancer types across the affected population. Cancer geneticist Edwige Kasper from Rouen University Hospital in France reported findings. She stated that some children developed two different cancers already. Others had passed away at very early ages.
Cancer cases among affected children
Medical Expert Perspectives
Clare Turnbull from the Institute of Cancer Research in London explained the situation. She described Li-Fraumeni syndrome as deeply concerning for affected families. The diagnosis creates a lifelong burden of cancer risk management. Families face devastating emotional consequences from this revelation.
Professor Allan Pacey from the University of Manchester expressed his sympathies. He noted the donor gave samples in good faith without knowledge. The donor remained completely unaware of his germline mutation. Standard screening would not have identified this exceptionally rare condition.
Professor Dorothy Bennett highlighted the current capabilities. Now that identification has occurred, screening becomes readily available. Children can undergo testing to determine their genetic status. Those inheriting the mutation require very regular cancer screening protocols throughout life.

Clare Turnbull described Li-Fraumeni syndrome as deeply concerning
Regulatory Gaps and Oversight Issues
No international law restricts how many times donor sperm reaches worldwide distribution. Nations maintain individual regulations about domestic donor usage limits. These regulations prove inadequate for controlling international distribution networks. The investigation revealed that some national laws were breached.
Belgium’s maximum of six families per donor was violated substantially. The European Sperm Bank acknowledged overusing this particular donor’s samples. The bank expressed its deepest sympathy to all affected families. Officials stated the mutation could not have been detected through available screening methods.
Also Read: Australians Applying For US Visa May Face Tougher Checks
Future Genetic Screening Implications
Professor Mary Herbert from Monash University in Melbourne emphasised urgent needs. More thorough genetic screening of sperm donors requires implementation. Stringent regulations limiting children per donor must achieve enforcement. The investigation demonstrates critical gaps in current oversight systems.
The incident represents an exceptionally rare convergence of events. The donor’s sperm carried mutations for an extremely rare genetic condition. Li-Fraumeni syndrome affects fewer than one person per 10,000 globally. The sperm was used an extraordinarily large number of times for conception.
Current Status and Response
The European Sperm Bank immediately blocked the donor upon confirmation. All affected children require ongoing screening for cancer development. Those inheriting the mutation face 50 percent odds of passing it to future offspring. Affected families received genetic counselling services regarding implications.
At least 197 children were conceived using this donor’s sperm. The actual number could prove significantly higher as data becomes available. Not all countries have yet submitted complete information regarding affected cases. Medical authorities continue investigating the full scope of this unprecedented situation.
This investigation highlights critical vulnerabilities in international fertility governance systems. Regulatory frameworks require strengthening to prevent similar incidents. Sperm banks must implement enhanced genetic screening protocols immediately. The incident serves as a wake-up call for the entire reproductive medicine industry worldwide.












